Written by Dr. Salvatore Giorgianni, PharmD and Armin Brott, MBA
Far too many American males are caught up in a storm of under-recognized, under-diagnosed, and poorly treated mental health issues, whose consequences play out in tragic headlines every day. They also play out—more quietly, yet more devastatingly—in homes and communities across the country.
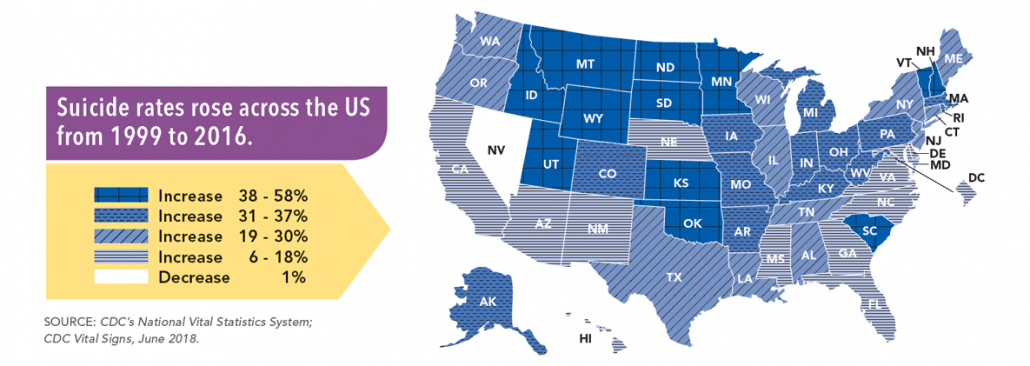
To get a sense of the scope of the problem, one need look only as far as the CDC’s most recent report on suicides in America, in which two statistics stand out. First, more than three-quarters (76.8%) of successful suicides in the US are committed by boys and men. Second, 83.6% of those successful suicides are committed by boys or men who had never been identified as having a mental health issue.
Suicide and Males
Multiple factors contribute to these two tragic numbers. To start with, annual wellness visits, which are mandatorily covered (for free) for women and girls under the Affordable Care Act (ACA), are not covered for men or boys. This contributes to yet-another sad statistic: overall, men are less than half as likely as women to have seen a primary care provider in the previous 12 months. Each of these non-existent medical visits is a lost opportunity to identify important physical and mental health issues.
Read: HOW TO GET MENTAL HEALTH CARE WHEN YOU’RE BROKE
And even if a man or boy with mental health issues were to have an annual physical, it’s unlikely that he would be diagnosed. Most primary care providers or those in the community (such as schools or the workplace) aren’t trained in the delicate art of identifying boys or men with mental health or depression. Men’s Health Network has done extensive research in this area, and to our knowledge, there are no good/validated tools to screen for mental health issues (in particular depression) in boys and men. Tools that are currently readily available to primary-care providers are either gender neutral or crafted with the female patient in mind. The startling lack of funding to develop male-centric tools, and the corresponding lack of research into the outcomes of such tools all but guarantees that men and boys with undiagnosed mental issues will continue to suffer without treatment.
Another factor that contributes to the problem of undiagnosed and untreated mental health issues in men and boys is that in American society, males have been socialized to view health—be it mental or physical—as someone else’s (typically women’s) domain. As a result, American males tend to show up in a healthcare provider’s office only in the direst of circumstances.
Regarding mental health issues, boys and men tend not to have social networks that allow, let alone encourage, dialogue between peers about emotional issues such as depression, anxiety, and isolation. And too often, when they do try to bring them up with a friend or loved one, they get ridiculed, dismissed, or receive some other type of verbal or non-verbal response that shuts down the conversation and makes them less likely to ever broach the topic again.
To address the mental health crisis facing the American male and our communities, we must develop strategies across the lifespan for loved ones, community institutions, health providers and civil authorities to better understand the gender-specific needs of men and boys that will enhance recognition of mental health issues and enable men to get help and treatment.
June is Men’s Health Month, making it the perfect opportunity for all stakeholders to rethink our approaches to mental health in men and boys and to provide much-needed direction, funding, and outreach to keep the brewing perfect storm from becoming even more dangerous.



No Comment